Issue 4 · Volume 55 · April 2023
Hormone and Metabolic Research 2023年第4期现已上线,欢迎免费阅读本期三篇精选论文。
Original Article: Endocrine Care
David SO et al.
The prognostic stratification of the current AJCC/UICC TNM classification for adrenocortical carcinoma (ACC) has been validated in only a few studies. In this study, it was hypothesized that redefining the T category cut-off would result in a significant improvement in estimated stage-related survival. In 935 patients with ACC from the SEER database, optimal cut-off values based on tumor size were first determined to redefine T1 and T2 categories. Cox proportional hazards regression analysis and receiver operating characteristics (ROC) were then used to determine the prognostic value of the revised version. A new cut-off value of 9.5 cm tumor size was established to differentiate between T1 and T2 tumors, leading to a revised TNM classification. As a result, a more homogeneous distribution of patients with ACC across all stages was observed. Notably, the predictive value of the newly proposed TNM classification in the ROC analysis exceeded that of the 7th and 8th editions of the AJCC/UICC classification system. Finally, the prognostic superiority of the revised TNM classification was confirmed in a multivariate Cox proportional hazards regression model. In conclusion, the present study demonstrates that updating the current staging system with revised T1 and T2 categories significantly improves the prediction of cancer-specific survival (CSS) in patients with ACC.

Original Article: Endocrine Care
Dong B et al.
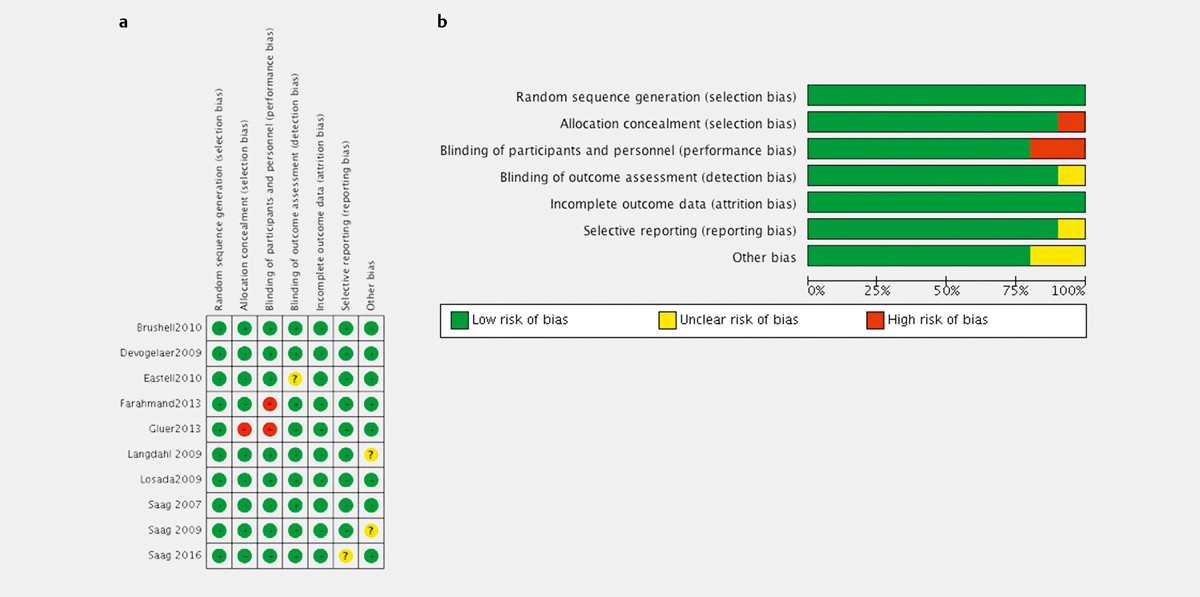
Osteoporosis (OP) is characterized as decreased bone mineral density (BMD) and increased risk of bone fracture. Secondary OP resulting from excess endogenous or exogenous glucocorticoid is defined as glucocorticoid-induced osteoporosis (GIOP). Current therapeutic strategies for GIOP are similar to menopausal osteoporosis, including calcium and vitamin D supplementation, bisphosphonates, and parathyroid hormone (PTH) analogues (teriparatide). Previously, several published meta-analyses compared anti-osteoporotic agents for the menopausal or aging-dependent OP. However, the physiopathologic bone metabolism of GIOP is different. In this study, we investigated the efficacy of BMD enhancement, bone fracture rate and safety of bisphosphonates versus teriparatide in the therapy of GIOP. We searched databases including PubMed, Embase, and the Cochrane Library until Jan 2023, and selected ten random clinical trials (RCT)s that compared the efficacy and/or safety of bisphosphonate versus teriparatide for GIOP patients. Teriparatide therapy increased lumber spinal BMD by 3.96% (95% CI 3.01–4.9%, p<0.00001), 1.23% (95% CI 0.36–2.1%, p=0.006) at total hip, and 1.45% (95% CI 0.31–2.58%, p=0.01) at femoral neck, respectively, compared to bisphosphonates at 18-month therapy for GIOP. Teriparatide also reduced bone fracture especially in vertebral bone (p=0.0001, RR 6.27, 95% CI 2.44–16.07), and increased bone formation and resorption marker levels. There was no difference in the incidence of adverse effects in bisphosphonate and teriparatide groups. Teriparatide showed better performance over bisphosphonate in BMD enhancement, bone fracture reduction, and bone remodeling improvement, without increasing the incidence of adverse effects.
Original Article: Endocrine Care
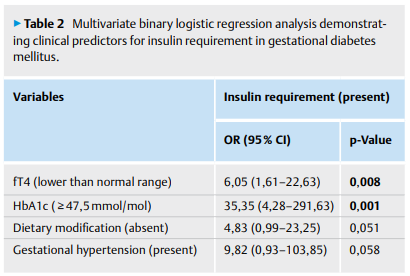
Topaloğlu Ö et al.
An insulin regimen may be necessary for about 30% of the patients with gestational diabetes mellitus (GDM). We aimed to investigate the association of free T4(fT4) levels with insulin requirement in pregnant women with GDM. We included pregnant women whose TSH levels were within the normal range and who were diagnosed with GDM, and excluded patients with thyroid dysfunction, chronic illnesses, or any previous history of antithyroid medication, levothyroxine, or antidiabetic medication use. The diagnosis and treatment of GDM were based on American Diabetes Association guidelines. Demographic features, previous history of GDM and gestational hypertension were recorded. Baseline (at diagnosis of GDM) fasting blood glucose, HbA1c, TSH, fT4, and fT3 levels were analyzed. We grouped the patients according to their baseline fT4 levels: isolated maternal hypothyroxinemia (IMH) (group A) vs. in the normal range (group B). We grouped those also based on insulin requirement in 3rd trimester. Of the patients (n=223), insulin requirement was present in 56, and IMH in 11. Insulin requirement was more frequent in group A than in group B (p=0,003). HbA1c (≥47,5 mmol/mol) and fT4 level (lower than normal range) were positive predictors for insulin requirement (OR:35,35, p=0,001; and OR:6,05, p=0,008; respectively). We showed that IMH was closely associated with insulin requirement in GDM. Pregnant women with IMH and GDM should be closely observed as regards to glycemic control. If supported by future large studies, levothyroxine treatment might be questioned as an indication for patients with GDM and IMH.