
Hormone and Metabolic Research 2021年第10期现已全新上线!我们为您精选本期三篇论文免费阅读。同时,欢迎您阅读本期更多论文,尽享医学之美。
Vulcan T et al.
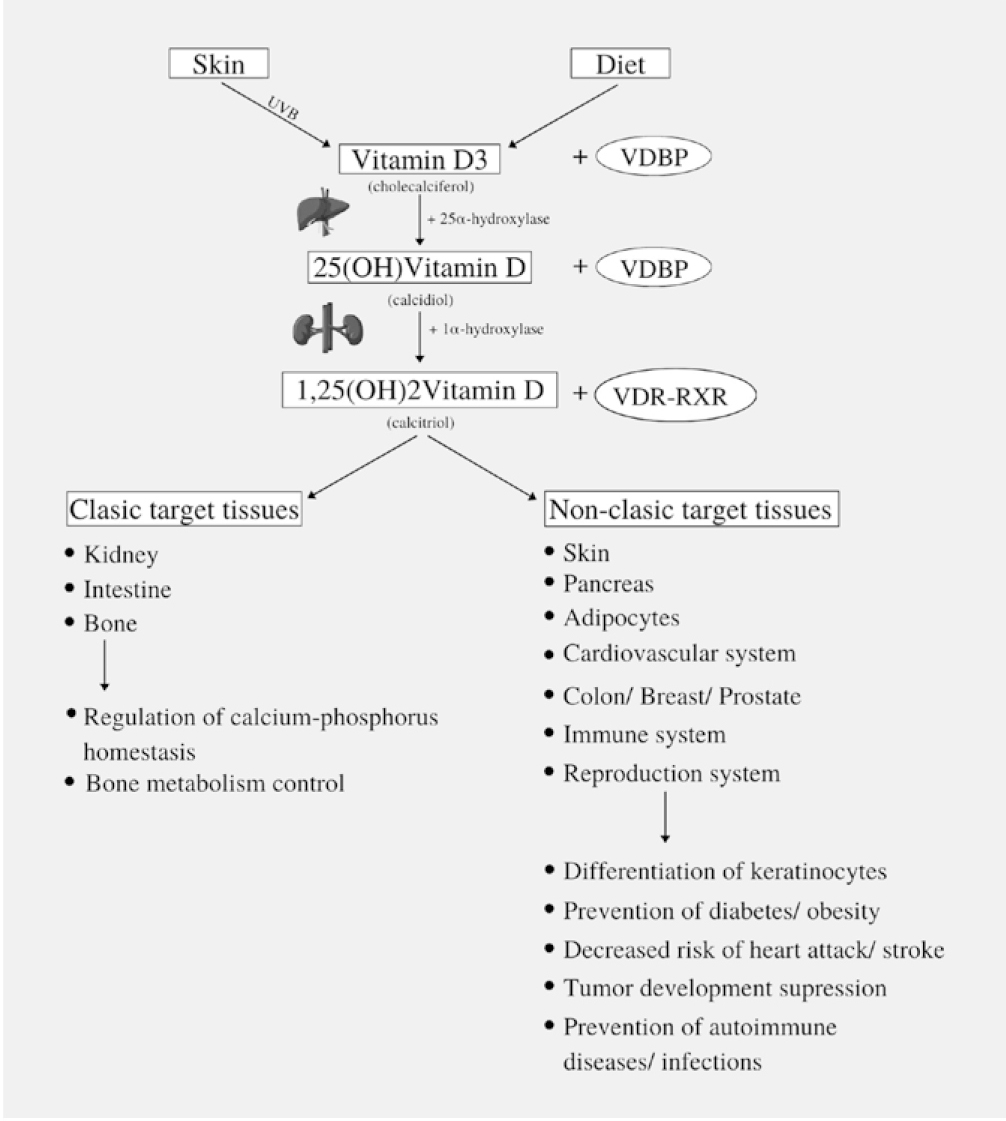
Polycystic ovary syndrome (PCOS) is one of the most prevalent endocrine disorder in women of reproductive age. Vitamin D and its receptor are thought to play an important role in PCOS susceptibility, although the impact of vitamin D receptor (VDR) polymorphisms on the hormonal and metabolic profile is still controversial. A literature search in PubMed and Embase was performed up to September 2020 for case-control studies in women suffering from PCOS, with outcome related to VDR polymorphisms effect on metabolic/endocrine disturbances. We have found 16 eligible studies including 2566 women with PCOS and 2430 controls. ApaI polymorphism seemed to be associated with hyperandrogenism in both Asian and Caucasian population. FokI variant was correlated with metabolic/endocrine parameters especially in Asian population, while a relation between Cdx2 genotypes and insulin sensitivity was observed in both ethnicities. VDR polymorphisms have an important role in PCOS development and related hormonal and metabolic abnormalities. Few case-control studies analysed the interaction between VDR variants and metabolic/endocrine parameters with the majority of the articles focused on the Asian region. Further research on various ethnic populations with larger sample size are still needed for a definitive conclusion, in order to allow early diagnosis and prevention of PCOS comorbidities.
Late Recovery of Parathyroid Function After Total Thyroidectomy: A Case-Control Study
Díez JJ et al.
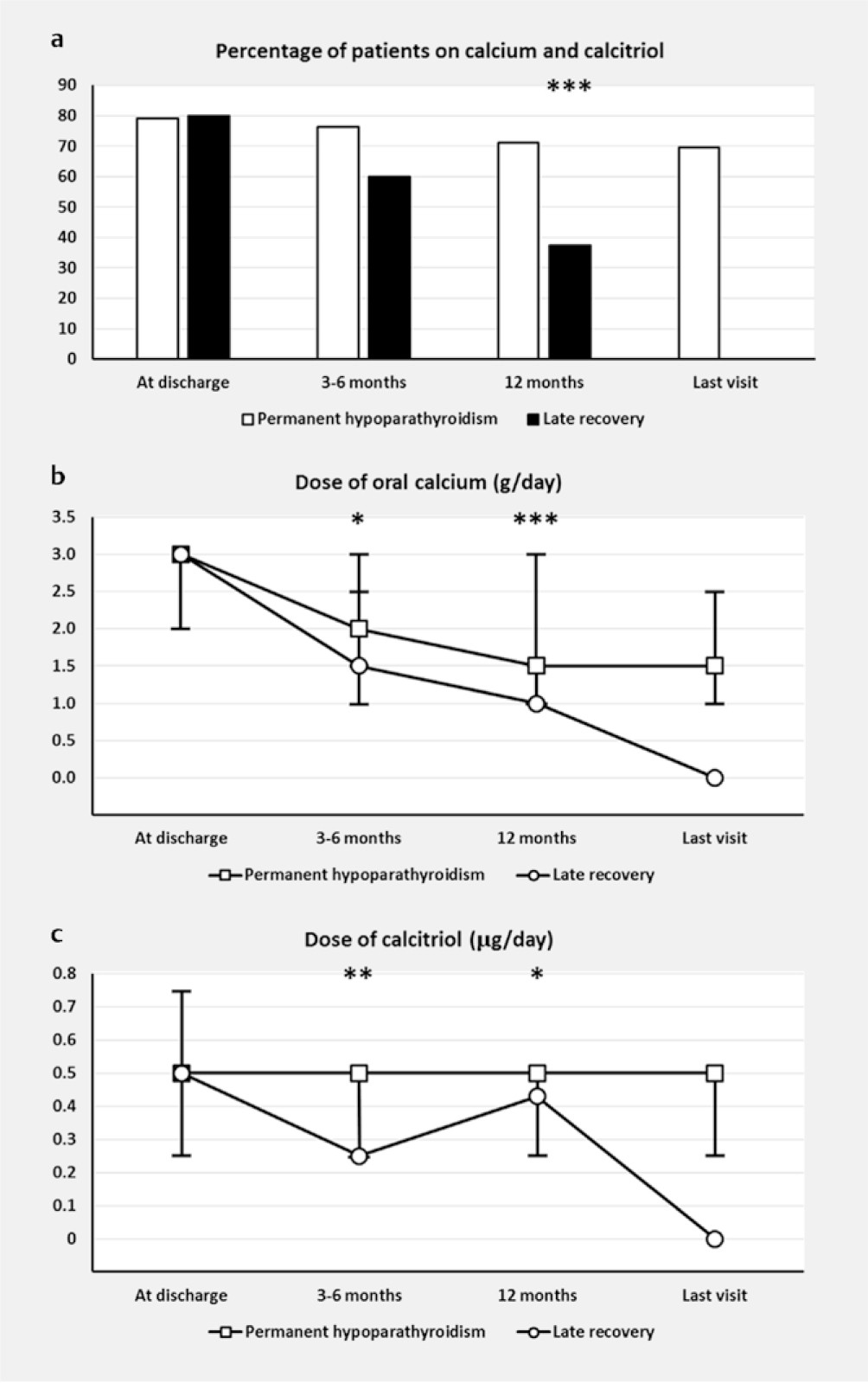
The clinical characteristics of patients with postoperative hypoparathyroidism who recover parathyroid function more than 12 months after surgery have not been studied. We aimed to evaluate whether the intensity of replacement therapy with calcium and calcitriol is related to the late recovery of parathyroid function. We compared the demographic, surgical, pathological, and analytical features of two groups of patients: cases, i. e., late recovery patients (those who recover parathyroid function>1 year after thyroidectomy, n=40), and controls, i. e., patients with permanent hypoparathyroidism (n=260). Replacement therapy with calcium and calcitriol was evaluated at discharge of surgery, 3–6 months, 12 months, and last visit. No significant differences were found in clinical, surgical, pathological, or analytical characteristics between cases and controls. The proportion of cases who required treatment with calcium plus calcitriol at 12 months was significantly lower than that found in controls (p<0.001). Furthermore, daily calcium and calcitriol doses in controls were significantly higher than those in cases at 3–6 months (p=0.014 and p=0.004, respectively) and at 12 months (p<0.001 and p=0.043, respectively). In several models of logistic regression analysis therapy with calcium and calcitriol at 12 months was negatively related to late recovery of parathyroid function. Although delayed recuperation of parathyroid function after total thyroidectomy is uncommon (13%), follow-up beyond 12 months is necessary in patients with postoperative hypoparathyroidism, especially in those whose needs of treatment with Ca and calcitriol are reducing over time.
Distinct Late-Night Salivary Cortisol Cut-Off Values for the Diagnosis of Hypercortisolism
van Baal L et al.
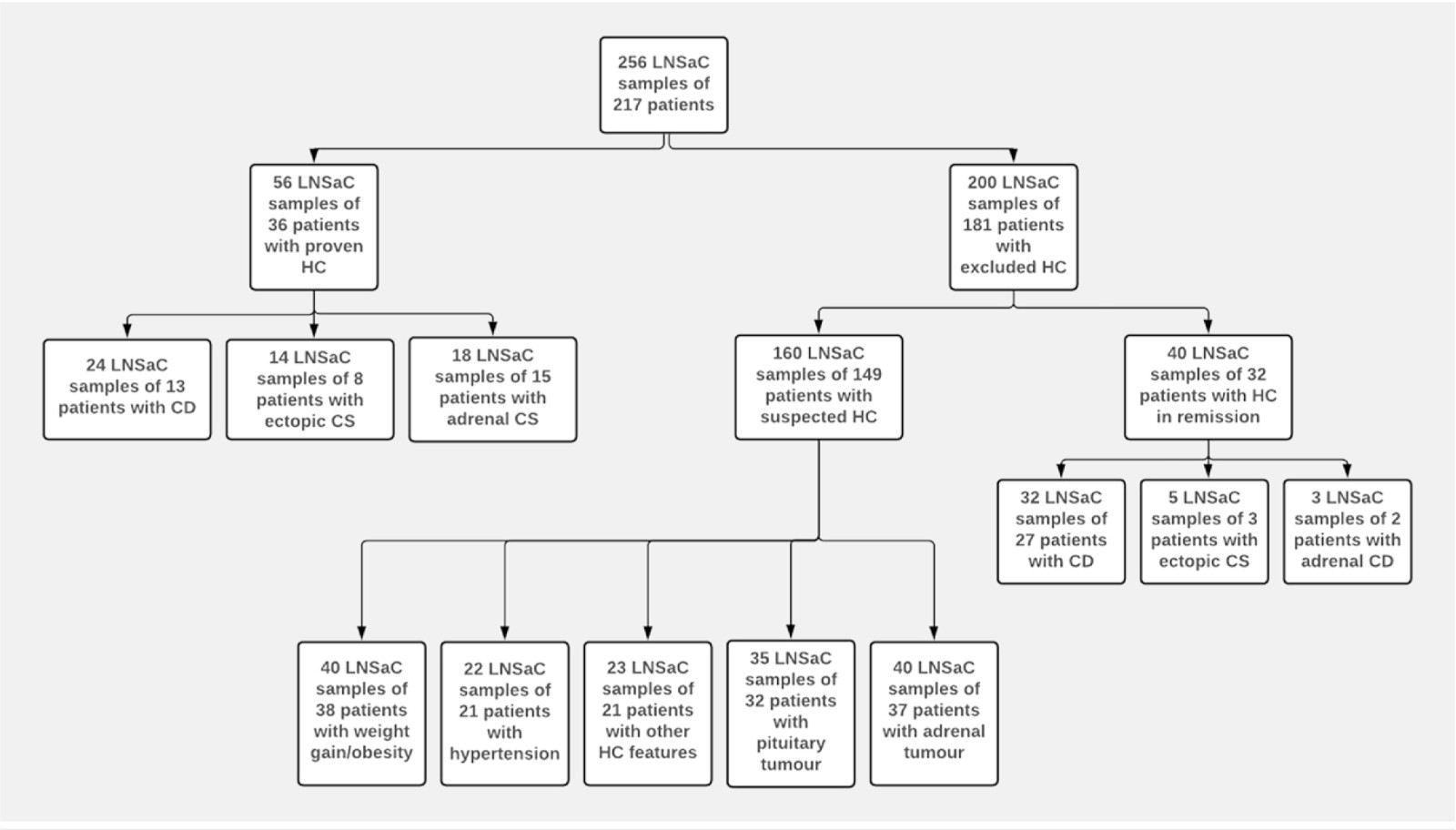
Due to high morbidity and mortality of untreated hypercortisolism, a prompt diagnosis is essential. Measurement of late-night salivary cortisol provides a simple and non-invasive method. However, thresholds and reference ranges differ among studies. The goal of this study was to define a threshold of late-night salivary cortisol for the diagnosis of hypercortisolism based on the used assay. Moreover, the influence of different aetiologies of hypercortisolism and individual comorbidities were investigated. Prospective analyses of 217 patients, including 36 patients with proven hypercortisolism were carried out. A sum of 149 patients with suspicion of hypercortisolism but negative endocrine testing and 32 patients with hypercortisolism in remission served as control group. Late-night salivary cortisol was measured using an automated chemiluminescence immunoassay. Cut-off values were calculated by ROC analysis. The calculated cut-off value for the diagnosis of hypercortisolism was 10.1 nmol/l (sensitivity 94%; specificity 84%). Only slightly lower thresholds were obtained in patients with suspected hypercortisolism due to weight gain/obesity (9.1 nmol/l), hypertension or adrenal tumours (both 9.8 nmol/l) or pituitary adenomas (9.5 nmol/l). The late-night salivary cortisol threshold to distinguish between Cushing’s disease and Cushing’s disease in remission was 9.2 nmol/l. The cut-off value for the diagnosis of ectopic ACTH-production was 109.0 nmol/l (sensitivity 50%, specificity 92%). Late-night salivary cortisol is a convenient and reliable parameter for the diagnosis of hypercortisolism. Except for ectopic ACTH-production, thresholds considering different indications for evaluation of hypercortisolism were only slightly different. Therefore, they might only be useful if late-night salivary cortisol results near the established cut-off value are present.
阅读本刊更多论文,请点击这里。
